HCMC NETWORK FEATURE: Patient’s chest opened to save life; MDs credit HCMC medical training
“My residency training made all the difference.”
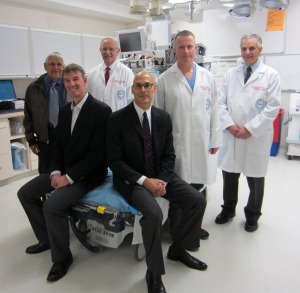
Photo 1: Drs. Eric Haug and Tom Wyatt (seated, left to right) recently returned to HCMC's Emergency Department to discuss dramatic save (back row, left to right, Dr. Ernie Ruiz, Dr. Joe Clinton, Dr. Rob Reardon, and Dr. Doug Brunette)
Although cracking open a chest in the Emergency Department makes for dramatic television, it does not happen every day. In fact, it was only recently reported that the procedure was used for the first time to treat post-ablation tamponade, which occurs when blood and fluid collect in the pericardial sac surrounding the heart and prevent it from pumping. In emergency situations, it’s critical that physicians are prepared to quickly assess, treat and stabilize patients. For emergency physicians Dr. Tom Wyatt and Dr. Eric Haug, their HCMC Emergency Medicine residency training prepared them with the clinical skills, the mental “checklists” and decision-making to opt for and successfully adapt a “go-for-broke” life-saving procedure.
Dr. Wyatt and Dr. Haug graduated together in 2003 and now practice at Mercy Hospital in Coon Rapids. Annals of Emergency Medicine issued a press release about their dramatic save, announcing the “First-Ever Emergency Department Thoracotomy for Post-Ablation Tamponade Reported.” The patient, a 42-year old woman, had collapsed and gone into shock. Dr. Wyatt described the case in the press release: “She was dying in front of us and we had exhausted every option in standard procedures…cracking someone’s chest open is a go-for-broke move that is normally only performed on patients with penetrating trauma, like gunshot wounds or stabbings.”
Drs. Wyatt and Haug were on duty at Mercy Hospital when the patient was brought in, unconscious. Using cardiac ultrasound, Dr. Haug quickly identified a large amount of blood around the heart. Due to clot, an ultrasound-guided procedure was unsuccessful in removing the blood and the patient became pulseless. Dr. Wyatt opened her chest, made a small incision into the pericardial sac and removed blood and clot; the patient’s pulse immediately returned. Due to the risk of uncontrollable hemorrhage, Dr. Wyatt and Dr. Haug stabilized the patient with repeated suctioning of blood and clot through the small incision and initiated massive transfusion to replace blood loss. After 65 minutes in the stabilization room, the patient was taken to surgery. She recovered and is doing well to this day.
Dr. Wyatt and Dr. Haug credited teamwork with highly skilled colleagues at Mercy Hospital as being critical for the successful outcome. Key assistance was provided by the cardiologist, echocardiography technician, resource nurse, pathologist, and others, until the cardiothoracic surgeon arrived and successfully repaired the patient’s heart.
“Emergency physicians do what we have to do to save a life, even if it’s unconventional,” explains Dr. Wyatt. “This patient had her chest open to the world for more than an hour, but she lived. My residency training made all the difference.”
What was it about their HCMC residency training that “made all the difference” that day? Dr. Wyatt explained that, “in a case like this, your training takes over because so many things are going on at one time. It’s almost like a reflexive nature, going down a checklist from our training of what to do next.” Innovative training in life-saving procedures began with Dr. Ernie Ruiz, who started the HCMC Emergency Department and was the first Residency Director, followed by Dr. Joe Clinton (now Department Chair) and Dr. Doug Brunette, who directed the residency program when Dr. Haug and Dr. Wyatt trained at HCMC (see Photo 2).
Dr. Haug also noted the importance of their extensive training in the use of bedside Emergency Department (ED) ultrasound, which was key for the rapid diagnosis. HCMC physicians were among the first in the world to utilize bedside ED ultrasound, starting in 1984 (see Photo 2). Since then, HCMC emergency physicians Dr. Dave Plummer, Dr. Rob Reardon (Photo 1) and others have pioneered in the use, research, and teaching of ED ultrasound diagnosis and ultrasound-guided procedures. Instruction has extended beyond HCMC to broad outreach training through curriculum development, textbooks, presentations at national and international conferences, and the Emergency Department’s educational website, hqmeded.com.
Impacts of this case continue as word of the procedure, the case report, and the HCMC ED residency have been posted on websites around the world. An Australian website that focuses on resuscitation posted a November 20 entry on their “Inspiration” page reporting “Emergency physicians from Minnesota (and graduates of the amazing Hennepin Emergency Medicine Residency) describe a patient who developed cardiac tamponade after an ablation procedure for dysrhythmia…” (see Photo 3).

Photo 3: Home page of RESUS.ME (Resuscitation Medicine Education), website by Dr. Cliff Reid, in Sydney Australia.
For more detail, see the next HCMC NETWORK FEATURE: Emergency Department Pioneered in Emergency Ultrasound Use and Continues to Lead Today, and check out the News page of HCMCImpact.org, to read about the statewide mission and services of HCMC.


