HCMC NETWORK FEATURE: Simulation — the next best thing to learning from a real patient
Here’s what Simulation training at HCMC looks like now and what’s coming.
Simulation is currently used at HCMC to train healthcare providers such as resident physicians and Emergency Medical Services (EMS) personnel. Simulation enables clinicians to practice procedural skills and management of critically ill “patients” in conditions that simulate clinical contexts, allowing them to learn and “practice medicine without risk.” Simulation training can also help to develop teamwork and communication, improve patient care and patient safety, enable exploration of medical errors, and develop systems expertise.
Plans are currently underway for a new 10,000 ft2 facility, the HCMC Interdisciplinary Simulation and Education Center. The first phase of this project, which will include 5,000 ft2, has a projected completion date in mid 2012. The new center will contain high fidelity simulation rooms with control rooms and debriefing areas, standardized patient rooms, a procedural skills room, and lecture facilities. In addition to clinical simulation training for diverse health care providers such as physicians, nurses, EMS providers and others, instructor training will be provided on developing, running and incorporating simulation into educational curricula.
In the simulation session shown below, in the current facilities, Dr. Danielle Hart, ED faculty physician and Director of Simulation, was assisted by two physicians and three nurses to train two four-person teams of ED residents.
Here’s how it worked: Each team ran two adult cases (1-motorcycle collision victim with pneumothorax and hemoperitoneum; 2-shock with both cardiogenic and septic components) and two pediatric cases (1-dysrhythmia, atrial fibrillation with WPW and subsequent V fib; 2-malrotation with volvulus). Debriefing sessions followed each case.
Note: Photos below illustrate actual case management: nothing was staged or posed.
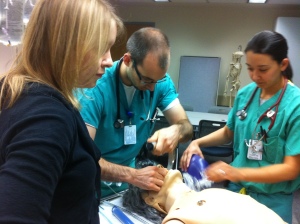
Staff prepare mannequin (photo 1) and set up (photo 2) for the motorcycle collision case. Faculty physicians facilitate the case from behind the two-way mirror and communicate with the nurse (through her earpiece) as she assists the team running the case. The mannequin has heart and breath sounds, with pulmonary and cardiac abnormalities audible through a stethoscope. The monitor displays ongoing vital signs as they change throughout the course of the case.
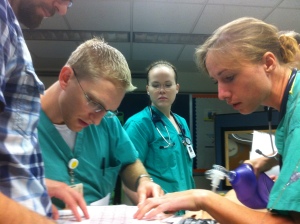
Team 1 runs the motorcycle collision case (photos 3 and 4) and interprets an electrocardiogram (ECG) (photo 5).
Meanwhile, facilitators behind the two-way mirror communicate through a walkie-talkie with the nurse (photo 6) and use the microphone to provide vocal responses from the patient to team members through a speaker in the mannequin. Facilitators adjust vital signs through the laptop computer, responding to actions taken and/or missed by the team as they run the case.
Team 2 intubates the shock case (photo 7).
Team 1 runs the pediatric dysrhythmia case and Team 2 de-briefs afterwards (photos 8 and 9).
Check back here for future features as work on the new Simulation Center begins.
For more information on simulation at HCMC, please go to the HCMC Simulation webpage
HCMC NETWORK FEATURES coming up? Read about hqmeded.com, the Emergency Department’s new educational website, and Dr. Smith’s ECG blog.